Understanding Septal Infarct: Causes, Symptoms, and Treatment
Septal infarct refers to damage or death of tissue in the septum, the wall separating the left and right ventricles of the heart. This condition occurs when there is an interruption in the blood supply to the septum, leading to a myocardial infarction (heart attack) in that specific area. In this blog post, we will delve into the causes, symptoms, diagnosis, and treatment options for septal infarct.
Causes of Septal Infarct:
Septal infarct is primarily caused by a blockage in one of the coronary arteries, the blood vessels that supply oxygen-rich blood to the heart muscle. The blockage is usually a result of atherosclerosis, the buildup of plaque within the arteries. Other factors that can contribute to septal infarct include:
a) Coronary artery spasms: Sudden contractions of the coronary arteries can reduce blood flow and lead to a septal infarct.
b) Thrombosis: Formation of blood clots within the coronary arteries can obstruct blood flow and cause a septal infarct.
Coronary artery embolism: When a clot or debris from another part of the body travels to the coronary arteries, it can cause a blockage and result in septal infarct.
Symptoms of Septal Infarct:
The symptoms of septal infarct may vary depending on the extent of damage and the location of the affected septum. Common symptoms include:
a) Chest pain: Patients may experience angina, a sharp or squeezing pain in the chest that can radiate to the arms, jaw, or back. The pain may be similar to that of a heart attack.
b) Shortness of breath: Due to the reduced pumping capacity of the heart, individuals with septal infarct may experience difficulty breathing or have a sense of breathlessness, especially during physical activity.
c) Fatigue: The heart’s decreased ability to pump blood efficiently can lead to feelings of exhaustion and fatigue.
Diagnosis of Septal Infarct:
To diagnose septal infarct, healthcare professionals employ various techniques and tests, including:
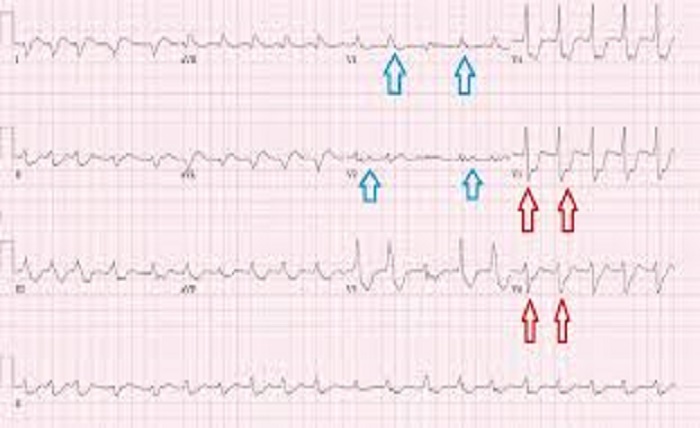
a) Electrocardiogram (ECG): This non-invasive test measures the electrical activity of the heart and can detect abnormal patterns indicative of a septal infarct.
b) Echocardiogram: By using sound waves, an echocardiogram provides detailed images of the heart’s structure and function, helping to identify areas of damage in the septum.
c) Cardiac catheterization: A thin, flexible tube is inserted into a blood vessel and guided to the heart to measure the blood flow and identify any blockages.
Treatment Options for Septal Infarct:
The goal of treatment for septal infarct is to restore blood flow to the affected area of the septum and prevent further damage. Treatment options may include:
a) Medications: Antiplatelet drugs, beta-blockers, and ACE inhibitors are commonly prescribed to reduce clot formation, lower blood pressure, and improve heart function.
b) Percutaneous coronary intervention (PCI): This procedure involves the insertion of a catheter with a balloon at its tip into the blocked artery. The balloon is then inflated to widen the artery and restore blood flow. In some cases, a stent may be placed to keep the artery open.
c) Coronary artery bypass grafting (CABG): In severe cases where multiple arteries are blocked, bypass surgery may be necessary. During CABG, a healthy blood vessel is taken from another part of the body and used to bypass the blocked artery, restoring blood flow to the heart.
Conclusion:
Septal infarct is a serious condition that requires prompt medical attention. By understanding its causes, recognizing the symptoms, and seeking timely diagnosis and treatment, individuals can improve their prognosis and reduce the risk of complications. If you experience any symptoms suggestive of septal infarct, it is crucial to consult a healthcare professional to receive appropriate care and guidance. Remember, early intervention can save lives and improve heart health.





